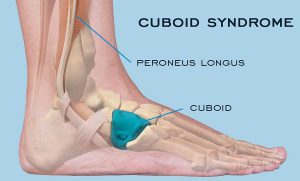
Cuboid syndrome is the result of injuries to the joints and ligaments surrounding the cuboid bone. This is one of the seven tarsal bones of the foot (talus or astragalus, calcaneus, navicular, cuboid and 3 cuneiform bones).
From a medical point of view, the condition is called a cuboid subluxation and occurs when the cuboid bone moves down and out, without being aligned with the calcaneus bone.
The cuboid syndrome causes pain in the external side of the foot, which can be confused with other conditions.
Clinical picture
Cuboid syndrome encompasses a variety of common symptoms and other conditions, sometimes making it difficult to diagnose. The most common symptoms include:
- Pain on the outside of the foot, which affects including fingers 4 and 5;
- Pain that aggravates the standing state, due to body weight ;
- Painful pain, dry or sharp and acute;
- Weakness and difficulty in walking and jumping;
- Redness, inflammation, and sensitivity in the injured area;
- Walking painkillers, to reduce pain;
- Reducing the range of movements of the foot and ankle.
Studies have reported that, in general, the cuboid syndrome is not uncommon in the population, but occurs most commonly in athletes and dancers. When the cuboid syndrome is correctly identified and treated, most people experience a complete recovery.
Causes
Cuboid syndrome can have different causes, but the most common are:
- Overload – this condition, along with injury, is most commonly seen in athletes and dancers. These groups of athletes tend to have intense physical activity, regardless of the presence of pain. Overload injuries tend to develop after long periods of intense activity, such as running;
- Ankle dislocation – ankle dislocation can also lead to injury to the Tarsus bones of the foot. A specialist study reported that about 40% of people with ankle dislocations or sprains can develop cuboid syndrome;
- Foot walking in pronation – people who develop this type of walking have a higher risk of having the cuboid syndrome because the muscles of the leg can pull the tarsal bones into abnormal positions;
- Other causes – climbing, uneven surfaces and sports involving fast and lateral movements, such as tennis, can cause the cuboid syndrome. Wearing shoes of poor quality or inadequate sizes may be another reason.
Also, if you do not take into account the indications of orthopaedic in Delhi regarding rest and recovery from a leg injury, various complications, including cuboid syndrome, may occur.
Diagnostics
The foot represents a complex, flexible and resistant segment of the body. It contains about 100 muscles, ligaments and tendons, 28 bones and 30 joints.
The complex structure of the foot and the non-specific nature of the pain within the cuboid syndrome make this injury difficult to diagnose.
Sometimes, medical imaging techniques such as X-ray or magnetic resonance imaging (MRI) do not identify signs of this condition, even if it is present. The cuboid syndrome may also mimic the symptoms of other foot problems, such as fractures or sprained heels.
In order to establish a correct diagnosis and to find the most effective treatment, the physician must perform a thorough physical examination and examine a person’s medical history.
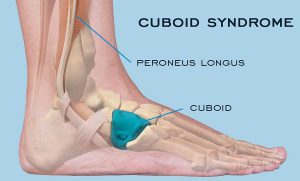
Treatment options
Treating cuboid syndrome always involves rest and elimination of activities that involve putting pressure on the injured leg. Applying ice and an elastic phase, but also raising the foot above the level of the heart on a pillow are other useful methods.
If the pain persists or worsens, the orthopaedic in Dwarka should be consulted urgently. Certain maneuvers performed by the therapists in the field can help to improve or eliminate the symptoms.
These maneuvers are meant to force the bone to return to its original position. However, it should be noted that such maneuvers are not recommended if there are other associated conditions, such as arthritis, bone disease, fractures, circulatory or nerve disorders.
Additional treatments may include the use of orthotics to support and properly align the foot, but also to administer anti-inflammatory drugs to reduce pain and inflammation.
In some cases, leg massage can help to reposition the bone. Surgery is used in rare cases when other treatment options have not worked.
Recovery
The length of time required for recovery from cuboid syndrome depends on several factors, such as:
- Duration of the treatment until the start of treatment;
- Cause of cuboid syndrome ;
- If the initial injury was mild or severe;
- If the instructions of orthopaedic in West Delhi were taken into account;
- If the condition has been correctly diagnosed and treated.
Physiotherapy in Dwarka can play an important role in the complete recovery of a person with the cuboid syndrome. Also, this therapy can prevent further complications.
Physical therapy includes:
- Reconsolidation of the strength and function of the foot;
- Maintenance of the muscles;
- Exercises to improve balance.
In some cases, to avoid pressure on the injured leg, the orthopaedic surgeon in Delhi may indicate the use of squats or walking sticks.
Risk factors
The common risk factors for the cuboid syndrome are:
- Overweight or obesity;
- Wearing shoes of inappropriate sizes;
- Wearing pairs of shoes of inferior quality;
- Practicing physical exercises without adequate heating;
- Practicing physical activities without taking into account pain and without having sufficient rest periods;
- Performing activities, such as running or walking on uneven or rough surfaces;
- Fractures of neighboring bones of the cuboid;
- Practicing sports such as athletics or ballet;
- Practicing physical activities that involve repetitive movements and increased impact on the foot;
- Association of other conditions such as arthritis or osteoporosis.
Perspective
Cuboid syndrome is not a serious condition and can be easily treated by the orthopaedic surgeon in Dwarka, sometimes involving physical therapy. The perspective is usually very good for people with this condition. Following treatment, most people can return to normal activities, with little risk of recurrence.
The orthopedic in Delhi should be notified if persistent pain occurs in the foot before doing any maneuver that could aggravate the situation.
Often there may be other health conditions that mimic cuboid syndrome. Rapid identification and early treatment of health status offer the best chances of recovery.