Introduction
Orthopaedic problems can affect people of all ages and can have a significant impact on their quality of life. Whether it’s a sports injury, arthritis, or a congenital condition, understanding the causes, symptoms, and treatments of orthopaedic problems is essential for effective management and long-term well-being.
Causes of Orthopaedic Problems
Orthopaedic problems can arise from a variety of causes, including:
1. Trauma: Accidents, falls, or sports injuries can result in fractures, dislocations, or ligament tears.
2. Overuse: Repetitive stress on joints, tendons, or muscles can lead to conditions such as tendinitis or bursitis.
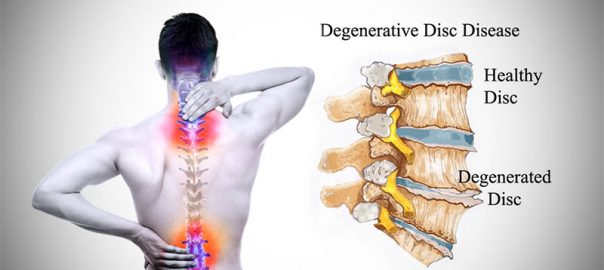
3. Age-related degeneration: As we age, the wear and tear on our joints can cause conditions like osteoarthritis.
4. Genetics: Some orthopaedic problems, such as scoliosis or clubfoot, can be inherited.
5. Infections: Certain infections can affect the bones and joints, leading to conditions like osteomyelitis or septic arthritis.
Symptoms of Orthopaedic Problems
The symptoms of orthopaedic problems can vary depending on the specific condition, but some common signs to watch out for include:
1. Pain: Persistent or recurring pain in the affected area, which may worsen with movement or activity.
2. Swelling: Swelling or inflammation around the joints or injured area.
3. Limited range of motion: Difficulty moving the affected joint or limb fully.
4. Instability: Feeling of joint instability or giving way.
5. Deformity: Visible changes in the shape or alignment of the affected area.
6. Weakness: Weakness or muscle atrophy in the affected limb or joint.
Treatments for Orthopaedic Problems
The treatment options for orthopaedic problems depend on the specific condition and its severity. Here are some common treatment approaches:
1. Non-Surgical Treatments:
-Physical therapy: Exercises and stretches to improve strength, flexibility, and range of motion.
– Medications: Pain relievers, anti-inflammatories, or injections to reduce pain and inflammation.
– Assistive devices: The use of braces, splints, or crutches to support and protect the affected area.
– Lifestyle modifications: Weight management, activity modification, or ergonomic adjustments to reduce stress on the joints.
2. Surgical Treatments:
– Arthroscopy: Minimally invasive procedure using small incisions and a camera to diagnose and treat joint problems.
– Joint replacement: Surgical removal of damaged joints and replacement with artificial implants.
– Fusion: Joining two or more bones together to stabilize a joint and reduce pain.
– Repair: Surgical repair of ligaments, tendons, or fractures to restore normal function.
Prevention and Management
While not all orthopaedic problems can be prevented, there are steps you can take to reduce the risk and manage existing conditions:
1. Maintain a healthy weight: Excess weight puts additional stress on your joints, increasing the risk of orthopaedic problems.
2. Stay active: Regular exercise helps strengthen muscles, improve flexibility, and support joint health.
3. Practice proper ergonomics: Maintain good posture and use ergonomic equipment to minimize strain on your joints.
4. Wear appropriate protective gear: Use protective equipment during sports or activities that carry a higher risk of injury.
5. Listen to your body: Pay attention to any pain or discomfort and seek medical attention if symptoms persist or worsen.
Conclusion
Orthopaedic problems can significantly impact your daily life, but with the right knowledge and treatment, you can effectively manage these conditions. Understanding the causes, recognizing the symptoms, and exploring the available treatments are essential steps towards a healthier and pain-free life. By taking preventive measures and seeking appropriate medical care from orthopaedic in Dwarka, you can minimize the impact of orthopaedic problems and maintain your overall well-being.