Arthritis affects the musculoskeletal system, specifically the joints. It is the main cause of disability among people over fifty-five years of age in Industrialised countries. However early arthritis treatment in Dwarka, West Delhi can relieve the symptom and makes people live a pain-free life.
Arthritis is not a single disease – it is a term that covers over 100 medical conditions. Osteoarthritis (OA) is the most common form of arthritis and generally affects elderly patients. Some forms of arthritis can affect people at a very early age.
The goals of arthritis treatment in Delhi is to control pain and other symptoms, minimize joint damage and deformity, slow the progression of arthritis, and maintain physical function. Arthritis treatment focuses on controlling pain, minimizing joint damage, and improving or maintaining function and quality of life. The goal of treating osteoarthritis is to reduce pain and improve the function of the affected joints.
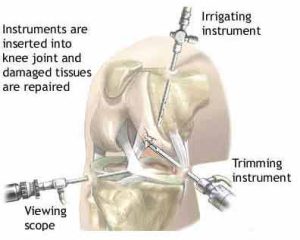
Joint pain and other symptoms caused by osteoarthritis can be treated without surgery, especially when the disease is diagnosed early. While joint surgery can relieve pain and improve joint function, recovery can be lengthy, requiring pain medication and weeks or months of physical therapy. Medical professionals usually only recommend surgery for some severe cases of arthritis. Surgery is used when the joint is severely damaged or when medication does not relieve pain and there is severe loss of function.
What causes arthritis?
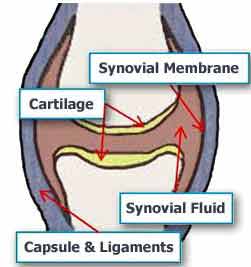
In order to better understand what is going on when a person suffers from some form of arthritis, let us look at how a joint works.
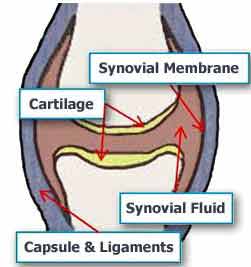 Basically, a joint is where one bone moves on another bone. Ligaments hold the two bones together. The ligaments are like elastic bands, while they keep the bones in place your muscles relax or contract to make the joint move.
Basically, a joint is where one bone moves on another bone. Ligaments hold the two bones together. The ligaments are like elastic bands, while they keep the bones in place your muscles relax or contract to make the joint move.
Cartilage covers the bone surface to stop the two bones from rubbing directly against each other. The covering of cartilage allows the joint to work smoothly and painlessly.
A capsule surrounds the joint. The space within the joint – the joint cavity – has synovial fluid. Synovial fluid nourishes the joint and the cartilage. The synovial fluid is produced by the synovium (synovial membrane) which lines the joint cavity.
If you have arthritis something goes wrong with the joint(s). What goes wrong depends on what type of arthritis you have. It could be that the cartilage is wearing away, a lack of fluid, autoimmunity (your body attacking itself), infection, or a combination of many factors. It is advisable to not avoid joint pain and meet the doctor for arthritis treatment in Delhi.
Does cracking knuckles cause arthritis?
Cracking the knuckles, also known as “popping”, is a kind of joint manipulation that produces a cracking sound. Cracking one’s knuckles is a deliberate action.
In fact, humans are able to crack several joints, including the ankles, shoulders, feet, jaws, toes, neck and back vertebrae, elbows, wrists, and hips.
Types of arthritis
There are over 100 types of arthritis. Here is a description of some common ones, together with the causes:
- Osteoarthritis – cartilage loses its elasticity. If the cartilage is stiff it becomes damaged more easily. The cartilage, which acts as a shock absorber, will gradually wear away in some areas. As the cartilage becomes damaged tendons and ligaments become stretched, causing pain. Eventually, the bones may rub against each other causing very severe pain.
- Rheumatoid arthritis – is an inflammatory form of arthritis. The synovial membrane (synovium) is attacked, resulting in swelling and pain. If left untreated arthritis can lead to deformity. Rheumatoid arthritis is significantly more common in women than men and generally strikes when the patient is aged between 30 and 60. However, children and much older people may also be affected.
- Gout – is a type of arthritis in which uric acid crystals deposit in joint and causes arthritis, most commonly affects males of 30 – 60 yrs and involves typically joints of the foot commonly the great toe.
- Ankylosing spondylitis – is arthritis involving the spine with or without major joints like the hip and knee. Commonly affecting young males of age 15-30 yrs.
- Post-traumatic arthritis – mostly after injury or fracture joint losses its alignment or damage to the cartilage which causes secondary osteoarthritis.
- Infectious arthritis (septic arthritis) – is an infection in the synovial fluid and tissues of a joint. It is usually caused by bacteria, but could also be caused by fungi or viruses. Bacteria, fungi, or viruses may spread through the bloodstream from infected tissue nearby and infect a joint. Most susceptible people are those who already have some form of arthritis and develop an infection that travels in the bloodstream.
- Juvenile rheumatoid arthritis (JRA) – means arthritis that affects a person aged 16 or less. JRA can be various forms of arthritis; it basically means that a child has it. There are three main types:
- Pauciarticular JRA, is the most common and mildest. The child experiences pain in up to 4 joints.
- Polyarticular JRA affects more joints and is more severe. As time goes by it tends to get worse.
- Systemic JRA is the least common. Pain is experienced in many joints. It can spread to organs. This can be the most serious JRA.
What are the signs and symptoms of arthritis?
Many patients who suffer from arthritis visit us for arthritis treatment in West Delhi with various symptoms. The symptoms of arthritis depend on the type of arthritis, for example:
- Osteoarthritis – The symptoms develop slowly and get worse as time goes by. There is pain in a joint, either during or after use, or after a period of inactivity. There will be tenderness when pressure is applied to the joint. Initially, pain may be only on stair climbing or standing from a sitting position. The joint will be stiff, especially first thing in the morning. The patient may find it harder to use the joint – it loses its flexibility. Some patients experience a grating sensation when they use the joint. Hard lumps or bone spurs may appear around the joint. In some cases, the joint might swell. The most commonly affected joints are in the hips, knee, hand, and spine ( in the spine it is known as spondylosis).
- Rheumatoid arthritis – The patient often finds the same joints in each side of the body are painfully swollen, inflamed, and stiff. The fingers( small joint of hands n feet), elbow, knee, and wrists are most commonly affected. Symptoms are usually worst on waking up in the morning and the stiffness can last for 30 minutes at this time. The joint is tender when touched. deformity also is seen which is diagnostic of it. Hands may be red and puffy. Many patients with rheumatoid arthritis feel tired most of the time. Weight loss is common.
- Gout – common symptoms are painful red swollen foot joints, especially the great toe. serum uric acid is generally high.
- Ankylosing spondylitis – common symptoms are stiffness in the back and neck with stooping posture associated with pain. most of the patients have HLA B27 positivity.
- Infectious arthritis – The patient has a fever, joint inflammation, and swelling. He will feel tenderness and/or sharp pain. Often these symptoms are linked to an injury or another illness. The most commonly affected areas are the knee, shoulder, elbow, wrist, and finger. In the majority of cases, just one joint is affected.
- Juvenile rheumatoid arthritis – The patient is a child. He will experience intermittent fevers which tend to peak in the evening and then suddenly disappear. His appetite will be poor and he will lose weight. There may be blotchy rashes on his arms and legs. Anaemia is also common. The child may limp or have a sore wrist, finger, or knee. A joint may suddenly swell and stay larger than it usually is. The child may experience a stiff neck, hips, or some other joint.
How will arthritis affect me?
Arthritis affects people in many different ways. How long the patient is affected and how severely it depends on the type of arthritis. Arthritis sufferers will find there are good and bad days. Most patients with arthritis will suffer from discomfort, pain, stiffness, and/or fatigue. Most important they gradually find difficulty in doing daily activities of living.
You may also feel frustrated that you are no longer able to grip things so well or get around like you used to. It is important to remember that if you suffer from arthritis this does not mean you have to give up having an active lifestyle. With proper arthritis treatment in Dwarka, West Delhi, and some changes to your way of life, there is no reason why you cannot continue being active.
Goals of Arthritis Treatment in Delhi
The goal of treatment is often to limit pain and inflammation and help maintain joint function. The goal of these strategies is to reduce joint stress and inflammation to relieve pain and slow the progression of arthritis. While many other treatments for osteoarthritis can reduce symptoms, they cannot effectively reduce joint stress and arthritis progression. Doctors may prescribe medications to relieve arthritis pain, but they also often recommend natural treatments.
While medications are only one option for arthritis treatment, they can relieve pain (and slow joint damage in many cases of inflammatory arthritis). These drugs are still used in the treatment of inflammatory arthritis, but on their own may not be enough to adequately control symptoms and limit the damage that inflammatory arthritis can cause. Anti-inflammatory and pain medications can relieve the symptoms of arthritis. These medications can help relieve pain and reduce inflammation in the joints at the same time, although they do not prevent rheumatoid arthritis from progressing over time.
Options for arthritis treatment in Dwarka include medication, lifestyle changes, joint injections, surgery, and more. While there is no cure for rheumatoid arthritis, early treatment and support (including medications, lifestyle changes, supportive care, and surgery) can reduce the risk of joint damage and limit the effects of rheumatoid arthritis. The goal of rheumatoid arthritis treatment in Delhi is currently to reduce the level of arthritis activity and remission as much as possible while minimizing joint damage and improving physical function and quality of life.
Heat and Cold Therapy
Heat and cold therapy can help reduce the pain and inflammation of arthritis. Using heat, such as applying heating pads to sore joints, taking hot baths or showers, or soaking warm paraffin in sore joints, can temporarily relieve pain. Pain can be relieved by applying moist heat (a hot bath or shower) or dry heat (a heating pad) to the joint. Thermal treatments may include long showers or hot baths in the morning to relieve stiffness, and use of an electric blanket or wet heating pad to relieve discomfort at night.
Using a cold compress, such as an ice pack on a sore muscle, can relieve pain and inflammation after strenuous exercise. Arthritis in certain joints, such as the knee, can be improved with a type of treatment called viscous supplements.
Physical therapy
Physical therapy is often recommended by doctors to help people with arthritis overcome some problems and reduce movement restrictions. Dr Ashu Consul may recommend physical therapy to help manage some of the symptoms of arthritis.
Diet
There is no specific diet for arthritis, but certain foods can help reduce inflammation. Doctors have found that treating depression with antidepressants and other therapies can reduce not only depressive symptoms but arthritis pain as well.
DMARDs are slow-acting antirheumatic drugs that help stop disease progression and joint damage in some forms of arthritis. Disease-modifying antirheumatic drugs (DMARDs) and biological therapies can slow or stop arthritis, which causes swelling in the body.
Short-term pain and inflammation relief may include pain relievers such as acetaminophen, aspirin, ibuprofen, or other NSAIDs. Oral pain relievers such as acetaminophen were the first common treatment. Over-the-counter pain relievers such as acetaminophen (Tylenol, etc.), ibuprofen (Advil, Motrin IB, etc.), or naproxen sodium (Aleve) may help relieve occasional pain caused by activities that do not use muscles and joints pain. – It’s like gardening indoors in winter.
How to avoid arthritis?
As most common arthritis is osteoarthritis which is mostly due to an inactive lifestyle. So by doing the following, we can save our joints
- Walking- daily walking nourishes our joint cartilage (ends of our bones) so maintains its elasticity.
- Daily exercise – daily exercise helps in maintaining our muscle strength around the joint so less stress goes to the joint and also adds to your bone mass (stronger bones).
- Avoid prolonged sitting – as sitting is a new disease in itself so avoid sitting more than 45 minutes at a time, get up and take a walk, sitting causes twice the stress on the joints of the spine and knee than standing.
- Healthy diet – as calcium-rich food gives minerals required by bones and joints.
- Maintain a healthy weight – as obesity increases the load on joints and causes degeneration (wear and tear).
- Early consultation – if u feel any joint/s is painful then seeing an orthopaedic doctor in Delhi will save u from later complications.
The Neo Orthopaedic Clinic
31 A, Pkt-II, Sector – 6 Dwarka, New Delhi 110075 India
Phone: 011-45020554
Secondary Phone: 9871442963
| Monday |
5:00 PM – 8:00 PM |
| Tuesday |
5:00 PM – 8:00 PM |
| Wednesday |
5:00 PM – 8:00 PM |
| Thursday |
5:00 PM – 8:00 PM |
| Friday |
5:00 PM – 8:00 PM |
| Saturday |
5:00 PM – 8:00 PM |
| Sunday |
Closed |







 Basically, a joint is where one bone moves on another bone. Ligaments hold the two bones together. The ligaments are like elastic bands, while they keep the bones in place your muscles relax or contract to make the joint move.
Basically, a joint is where one bone moves on another bone. Ligaments hold the two bones together. The ligaments are like elastic bands, while they keep the bones in place your muscles relax or contract to make the joint move.